That Sinking Feeling... It Might Be Prolapse
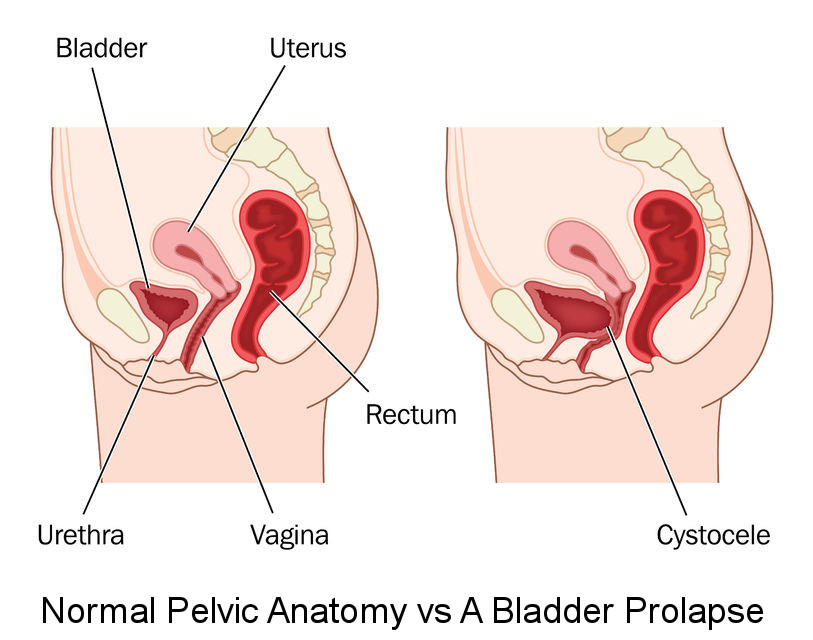
Pelvic organ prolapse is a common problem for women. It involves one or more of the pelvic organs dropping down from its usual position in the pelvis. This creates a bulge or lump in the vagina, and can give a feeling of sinking or heaviness down below.
Women may experience a bladder prolapse (also called a cystocele), a bowel prolapse (rectocele) or the uterus itself can prolapse (or the top of the vagina if you have had a hysterectomy). Some women have a combination of 2 areas, or even all 3 areas, descending.
Can prolapse happen to me?
Yes! About half of all women who have ever had a baby have some level of prolapse, although only about 20% of women are symptomatic enough to seek treatment. Certain factors increase your risk of prolapse, such as family history, delivering a large baby and forceps deliveries. However, some women who have never had a baby can also develop prolapse, especially if they are very overweight and have done a lot of heavy lifting over their lifetime.
Read Debbie’s story (1) to understand how prolapse can impact your life:
I never thought I would be the kind of person who would get a prolapse. Yes, I had had 3 pretty big babies - all over 8 pounds in the old scale, and I remember the first one was a very long labour. The doctor had to use forceps to get him out as he got stuck, and I had lots of stitches. But that was years ago. My children are now in their 30’s and 40’s and have children of their own. I never had problems with bladder leakage after my children were born, and I have always been pretty active and healthy.
I first noticed problems a few months ago. I went to clean myself in the shower one evening and felt a lump just inside my vagina. I completely panicked. Thoughts of cancer raced through my head. I couldn’t see my GP fast enough the next day. I was incredibly relieved to find out it wasn’t cancer, but really surprised when she told me I had a bladder prolapse. My GP recommended I see a Gynaecologist.
It was a bit of a wait to see the Gynaecologist. In the meantime, I started noticing my prolapse more and more. It always seemed to be there by the end of the day, and sometimes I could feel it by lunchtime. Then I started having trouble with my urine. I sometimes felt like my bladder wouldn’t empty properly, and I started to feel like I had to go more often, especially at night. I had never had to get up to the toilet overnight, and now I was getting up once or sometimes twice, every night! To my embarrassment, I even wet myself a few times just out of the blue. I suddenly felt like an old lady, and I started wearing pads just in case. It was so embarrassing having to buy continence pads in the supermarket.
When I finally saw the Gynaecologist, he confirmed I did have a bladder prolapse, but that it was still relatively minor. He recommended I see a Physiotherapist. The Physio got me started on pelvic floor exercises and showed me a few tricks to empty my bladder properly. She also recommended I try a pessary. I wasn’t sure, but after thinking about it, decided I had nothing to lose. The pessary really helps. It holds my prolapse up, so I don’t feel the lump. Since starting treatment I can now empty my bladder properly again, and I am not wetting myself anymore, or getting up at night either. It’s such a relief.
How can prolapse be treated?
Traditionally, treatment for prolapse has involved surgery. However, up to 30% of women who have prolapse repair surgery develop a recurrent prolapse. Certain past surgical methods of prolapse repair using vaginal mesh have also received a lot of attention recently, as about 10% of women developed severe complications, including chronic pelvic pain and mesh erosion. This type of mesh and surgery are now banned in Australia. Surgery can still be a good option for many women, particularly if they have a more severe prolapse.
There is now increasing evidence showing the benefit of conservative management for prolapse, especially when treated early. Conservative management includes pelvic floor muscle exercises, improving any lifestyle factors which may be making the prolapse worse, and fitting a support pessary. A Women’s Health Physio can offer these kinds of treatments. Even if you do opt for surgery, it is still helpful to see a Physio before and after surgery in many cases, to prepare you for the surgery and to help in your recovery.
So if you find an unexpected lump in the vagina, it’s good to know help can be found.
Always seek professional medical advice if you find new lumps or bulges or develop new symptoms.
(1) Not her real name.
